Education and Exercise
We try to identify which environmental and lifestyle factors may be contributing to a problem. Gaining an understanding can facilitate healing. Exercise has many benefits, ranging from increasing collagen production in weak tendons and ligaments, to building bone and muscle to preventing falls and injuries.
Shock Wave Therapy
Shock wave therapy can provide an exercise stimulus to tissues when the person is unable to exercise because of pain or other disability. Shock wave therapy can help resolve chronic myofascial and tendon problems and is being researched to facilitate recovery from muscle injuries and for its anti-inflammatory effects. Shock wave therapy is performed once a week for 4 to 6 weeks.
Classic Injections
Classic injections for musculoskeletal disorders and entrapped nerves have traditionally employed corticosteroids, which shrink swollen tissues and create space for healing. Corticosteroids are useful in conditions involving excessive pressure in the carpal tunnel, shoulder impingment and spinal stenosis (compressed nerves in the spine). For some conditions, a simple combination of local anesthetic and dextrose – a sugar, same as glucose, typically used in IV fluids – triggers a local healing response.

Biologic Interventional Techniques
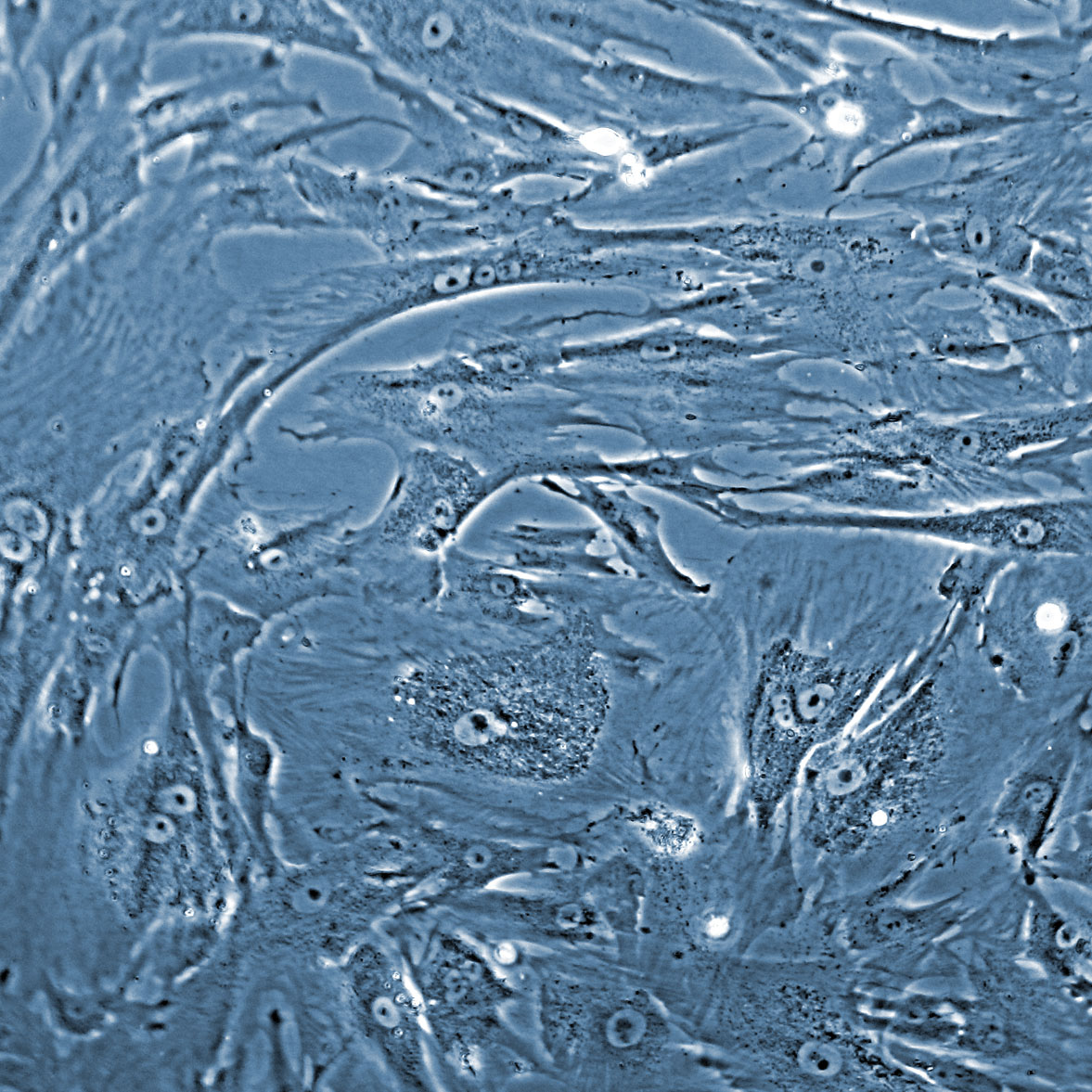
The most common biologic interventional techniques involve platelet-rich plasma (PRP) and bone marrow aspirate concentrate (BMAC). Platelets injected into degenerated tissues are able to heal tears and initiate a regenerative response. Since 2013, the Bodor Clinic has had a 70% success rate for good to excellent results in the cervical, thoracic and lumbar spine. In 2020, Ryan Dregalla PhD, Yvette Uribe BS and Dr. Bodor published on how BMAC injected into disc material was capable of synthesizing hyaluronic acid, the gel in cartilage and discs. In 2021, they published on the safety and efficacy of combining PRP with local anesthetics to optimize patient comfort. Ongoing studies include using BMAC to heal the torn ACL, for which using a special ultrasound-guided technique the team is having a 90% success rate at restoring at least one bundle of the torn ACL and an 89-92% scores on the KOOS at 1 year. BMAC is most often used for osteoarthritis.

Ultrasound-Guided Surgery
Mini-open and arthroscopic carpal tunnel releases have provided the fastest recoveries and best outcomes. Now carpal tunnel release can be done even less invasively, with the camera (ultrasound transducer) on the outside, providing an even faster recovery and best final outcome. We perform ultrasound-guided surgery for vaccination-related shoulder dysfunction, calcific tendonitis, tendon contractures and exertional compartment syndrome.
